North Lanarkshire
24 September 2014 – Fourth meeting of the group
Here’s our Programme for the day.
Goals for the day:
- Revisit community mapping and effective communication
- Develop and agree improvement ideas to trial
- Agree homework and next steps
Connecting up
Music is a great connector. Our icebreaker – to get everybody talking, relaxed and to get to know each other just that bit little more – was to get group members to talk in pairs about their favourite songs. I think we repeated this 3 times. People had great fun revealing why, for example, Eric Clapton’s ‘You Look wonderful Tonight’ was so special to them or what it was about Queen that they loved and their experiences of seeing them live. I also loved finding out that Louise’s family had Team B songs to keep them gee-ed when they needed to be. Brilliant!
Rikke was in her element as DJ, finding some of them on spottily or youtube for the bigger group to listen to and share.
Last session’s homework – feedback from group
OK, this lasted WAY beyond the time allotted in our programme. However, I decided to let it run as I thought it useful to let the group hammer out some of these issues. It seemed to help them really decide what were the most crucial things they wanted to focus on during the rest of the day. However, it left Rikke and I as facilitators a bit stressed as we had to adapt and re-jig the programme to accommodate this!
The homework as based around the idea that online resources for people with heart failure are not particularly good. The good gets mixed in with the bad and the accurate with mis-information. Also:
- It’s often hard to find through online searches/not known about
- People not signposted to relevant info
- It’s too negative/scary!
- It’s too full of jargon
- It can be very confusing eg. American-based or out of date or, as already mentioned, downright wrong!
Effectiveness of different search terms?
- If you search for ‘Heart’ alone in North Lanarkshire Council website this brings up schools etc. It’s not until about the 5th line that you get anything relevant.
- North Lanarkshire Council search for ‘heart disease’ brings up events eg on fundraising, and not links to heart condition.
- ‘Heart’ is used as a prefix for many things! Also Hearts football club.
- Information is only as good as what goes in (if information is poor, a loss of credibility results).
Resources we like:
- Chest Heart and Stoke resources – with one describing their newsletter as a ‘saviour’ with practical information
- British Heart Foundation resources
- Cardiomyopathy Association resources
- ‘Patient part’ of European Society of Cardiology
- Heart Failure Matters website, informed (?) by support groups with heart failure (with links to British Heart Foundation)
- Agreed that links from trusted websites (such as Chest Heart and Stroke and British Heart Foundation) to others provides quality assurance
- Ones without jargon and clear layout
Resources we don’t like- and things we want more of
- Resources that aren’t welcoming
- Ones that are too clinical (even the ‘good ones’ can be too clinical sometimes)
- NHS resources cited as the most negative – ‘very scary’ or boring!
- We want to learn more from others’ experiences
- People can have different personal experiences- but there are also strong similarities in issues faced eg poor experiences with GPs and late diagnosis (a recurring theme); heart failure patients are often angry at diagnosis; services don’t talk to each other in the NHS/they are fragmented.
- Good to have different resources for different people at different times eg Facebook, doctors, meetings with others
- We’d like:
- Joined up pathways
- A one-stop shop?
Our group’s experience- and what they think is most important!
Heart failure is not a disease, but a response to something else. The current situation has to change to achieve earlier diagnosis and appropriate support. This has become the key issue for our group.
The group feel that GPs need to be the lynch pin for person-centred care, ‘but they don’t look into your medical history properly’ – so people may not be properly diagnosed and medically managed (and may even be on the wrong medicines)! ‘GPs aren’t joining the dots!’ This is made worse by there being ‘lots of wrong information out there!’ ‘Fluid on legs’ may lead you to a self-diagnosis of heart failure, but it may be other things and not be heart disease (although the information doesn’t tell you this). Louise B spoke of her husband’s heart failure being missed time after time. ‘He passed all 6 tests- maybe because he was a fit guy’. It was only by going to the British Heart Foundation who gave him a table tilt test, that he finally got a diagnosis (and a pacemaker before it was too late)!
Clearly, fear can be a barrier to get people to go to their GP too! We need accurate information, a checklist even, without scaremongering people. We want to provide a positive message that if you do have heart failure there are things that you can do! And according to our group members, that shouldn’t automatically mean being advised to give up your job – that can lead to depression!
Often it’s only when people meet a heart failure nurse that things fall into place. However, the heart failure nurses can only do so much and are overstretched. Plus, their focus is not on prevention. By this point, things have advanced and we may have missed opportunities to stop things getting worse! Ian and Margaret’s own experiences of attending the cardiologist every year for 25 years was that there was little they could do for themselves that would make a difference. In hindsight, they believe this was not the case and they missed opportunities to keep themselves well to avoid going down the heart failure route. Margaret’s son, who has the same inherited condition, has the benefit of her hindsight and is keeping fit and on the right medicines.
Health literacy can also be a big problem. There’s no consistency around receiving written information and patients aren’t good at knowing the questions to ask!
Peer support can be really valuable, however, people also worry about being bullied and stigmatized if identified as a ‘heart failure’ person – just as young people who are obese worry about being seen doing exercises with other obese kids and may rather hide at home!
Is it all about better education?
In summary, are there three key aspects?
- Getting what we need from GPs- by training and challenging them
- Until then, making sure that people know they can turn to third sector organisations (like Chest Heart and Stroke and the British Heart Foundation) for advice and support and to get tips and support from ‘people like them’
- Public awareness raising to support earlier diagnosis
This led the group to identify what was needed, namely…….
How do we support or challenge GPs – and maybe practice nurses too?
- Through complaints
- Forum with GPs
- Small scale pilot –sharing success of this with others
- Training and educating GPs e.g. the British Heart Foundation said that they could offer training to front of house staff and GPs
- Tools to help challenge GPs eg list of questions to ask at appointment/pre-consultation resources to help empower people and/or prepare them before they go in to see the doctor. People shouldn’t be so passive and frightened to complain!
- We heard that in England GPs are being inspected-covering clinical practice to health promotion over next 3 years – this may be triggered by a complaint. A framework has been established to inspect on different things, with a scoring matrix used. They contact a cross-section of patients by telephone and may for example, select patients from the heart failure register and ask them how happy they are with their treatment.
- There was some preference from within the group for making greater use of nurses in GP surgeries; seen as an under-used resource who can provide support but also identify when you need to see the GP. They should be targeted too in any initiative/education drive/ training offer or ‘bundle’.
- Chest, Heart and Stroke’s Voices programme is designed to train and empower people.
- We can go to GPs with an offer of help? (There are different things we can offer that can help them).
- However, should we also be thinking about ‘What I want the GP to ask me?’
The group discussed that this is in the context of:
- Increased focus on self-management noted and how this all interacts with the different parts of the system
- More and more referrals from GPs to Social Work- signposting to them and to 3rd sector/party organisations.
- More people are being re-referred to GPs after initial ‘fobbing off’ Support groups in Scotland are patchy and focused on people at end of cardiac rehab
- Exercise is not something everyone is interested in. CHS are growing more social groups, incl. online Facebook ones.
- It’s also recognized that groups can be more generic eg focused on long term conditions and not just heart failure or that people may prefer to ‘get away’ from heart failure (especially if these become competitive or negative) and get involved in groups focused on their interests.
- Social Media
- Some groups are closed. Issue as to whether this identifies people with heart failure or not as online links can be traceable – some people don’t mind; others don’t want their neighbour to know they have heart failure.
- Some patient forums, including the British Heart Foundation’s, aren’t moderated. This means that people can post up ‘wrong’ information that goes unchallenged and can lead to spread of mis-information. Moderator needed?!
- Issue of online trolls
- Things not being joined up
- GPs are fearful of cardiologists? If a patient is diagnosed with an acute condition by a cardiologist, the GP won’t see the patient as ‘no longer under primary care.’
- The heart failure nurse isn’t copied into all correspondence – so may need to investigate certain things him/herself regarding a patient’s care or condition.
- This can leave patients in a real predicament eg. if I lose my medicines, is it ok to miss them? Lack of certainty over who can tell me/give me advice on this and/or provide the medicine? In Chris’s case, pharmacists didn’t want to engage with him on this and the GP didn’t reply to the message left on the answerphone.
Revisiting community mapping
This part of the day was to explore the content and functionality of local information that was already available. As we’d already covered some of this ground during ‘homework feedback’ we focused our time on looking at some of the following sites – as possible inspiration for the work North Lanarkshire Council has undertaken to do around improving local online information for people with heart failure.
- East Dunbartonshire Assets map
- Google maps – free, slightly les sophisticated than above – lots of examples out there!
- Voluntary Action North Lanarkshire ( see Locator)
- Voluntary Action South Lanarkshire ( see Infobase and Locator search)
- ALISS
- Living it Up (Flourish) and its No Delays prototype which can be found from this page
- There’s also the Living it Up experience guide to ‘Living with heart failure’
Developing plans for what we want to pilot/trial
We started out from the basis that by the end of today we wanted to AGREE ideas that we wanted to test/trial. Ideally, a minimum of two and maximum of four, with responsibility for delivering them shared across the group and involving both professionals and non-professionals.
The group were reminded:
- To focus on what we can do (and not what we can’t)
- We have three months until the end of December to do this within the timeframe of the project
- No budget to support these ideas apart from our time, energy, commitment and expertise (unless project partners can provide or secure funding)
- Top 10 tips for Improvement
We also took some time to consider What we hope to achieve and earlier Potential Improvement Ideas and where we had got to last time. Rikke re-presented the ideas we had formed at the last session – with the opportunity to amend/delete or add to these.
Interestingly, the discussions we had had earlier that morning had really shifted on the group’s thinking – very much away from peer support groups for example, to focusing attention on achieving earlier diagnosis and raising awareness.
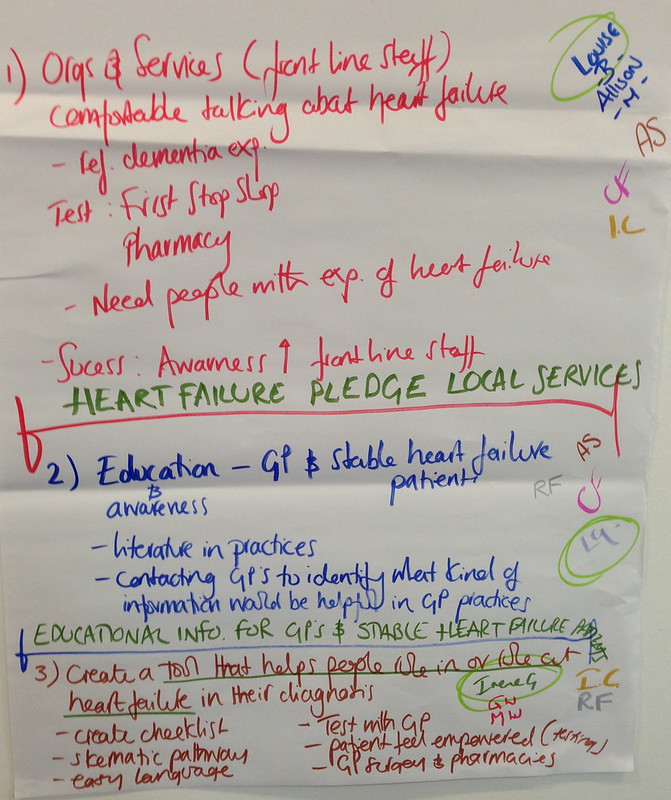
Next step – agreeing ideas to test and setting up working groups
These are the ideas the group came up with instead! We then asked the group to vote on their favourite. They were given four red dots each which they could allocate however the liked – so they could spread these among the three ideas or give them all to one!
At this stage we split the group up into three smaller groups to work on the three ideas identified! We asked them to complete the Template provided (after taking them through this). Each group was then asked to provide feedback to the bigger group – sharing their plans and inviting comment, feedback and taking the opportunity to ask for any extra help they needed!
The ‘missing’ fourth idea, will be improvement of North Lanarkshire Council’s online resources, working with individuals in the group to improve local information.
Last, but not least, we invited people to allocate themselves to a Working Group to take these ideas forward from planning into implementation. People were encouraged to be on more than one Working Group if they wished. So, they were free to reassign themselves following feedback if they had energy and enthusiasm for an idea.
Homework and plan for next meeting
As homework we encouraged each group to be in touch before the next session (on 29 Oct) – physically or by email to try and takes plans forward.
As for the next meeting, we felt this should include
- reports from each Working Group on progress
- focus on how to measure impact and learn from any tests of improvement
- how to share/spread improvement ideas to others
The group was happy with this but wanted to include what would happen at the end of the project to the programme.
Feedback and evaluation
All smiley faces (10 out of 10 folk). Sorry I didn’t get everyone into the picture!
What went well?
- The soup was lovely!
- Feedback on the homework from the last session was really valuable
- Good to have British Heart Foundation there too!
- Good balance in group between professionals and non-professionals
- No TLAs (third letter abbreviations)
- We’ve moved forward.
- Interaction and talking
What didn’t work so well?
- Confusing tea bags!
- A bit cold in the room
- Wi-fi in building!
- The facilitators found going off the agenda, esp with regard to timings stressful, but group members welcomed this and the flexibility
- Less parking than lst venue (but no stairs which is good)
What will you take away from the day?
- Feeling rejuvenated!
- We have actions plans!
Chest Heart and Stroke want your feedback
Chest, Heart and Stroke are inviting feedback on two options for their new look newsletter: Newsletter 1 and Newsletter 2 (or options 1 and 2). The deadline is Friday 3rd October, so get your views in quick by completing this survey!
OPTION 1
OPTION 2
20 August 2014 – Third meeting of the group
Here’s our Programme for the day.
Goals for the day
- To map our community assets
- To introduce approaches to improvement
- Develop improvement ideas to trial
- Agree homework and next steps
Connecting up
Our plan had been to get the group to share in pairs (then move onto a new partner) top tips for staying well. However, we had a few drop outs, several last minute. We only found out on the day that one of our group was being treated for another illness, but would return to the group next time. Another had suffered a close bereavement and would most likely not be returning to the group. This meant we were down to three people with lived experience of living or caring of someone with heart failure. Some of our professionals who had made it to the two previous sessions couldn’t make it either: one was on holiday and the other person’s duties had changed so she now saw patients on Wednesdays – the day of our sessions.
This meant we were down to eight on the day, when we had hoped for 13 or 14. It’s easy to say, expect the unexpected and be prepared to be flexible – and we were. What’s less easy is dealing with the emotional impact of this as a group and as individuals….
As for myself, I wanted to let the group know that I was pregnant with my baby due at the start of November. This meant that I would be with them for one more session. After that, one of my colleagues at IRISS would be taking over my role as project leader and co-facilitator for the group.
So…instead of working in pairs, we formed a circle by drawing our chairs together in a ring. We used this time to share what positive experiences we had experienced over the Summer, those that had made us feel positive about being alive and that we had drawn strength from. The two facilitators- Rikke and myself – were included in this. Should you always remain neutral and outside the group? Possibly not, as the group has a relationship with us too. We bring ourselves to every meeting, while conscious that it is the group’s job (not ours) to provide the content for discussions that will shape and drive forward what it is they do!
Sharing our stories felt very personal – at least it did for me – and was part of a process in building trust and relationships where boundaries become blurred and broken down. People later commented that they particularly liked this part of the day and preferred sitting in a circle. Strangely, we do that with the other Keeping it Personal group, not this one… Note to self…
Insert videos
We asked for permission to film and share these videos.
Recap on person-centred care and support: the power of pictures!
We felt it was important to ground people in what was understood by person-centred care and support before moving on in the day to identify improvement ideas we wanted to trial. Last time, we have devised a task to get people to come up with their own campaign, using the ideas and words to express these that were most meaningful to them. Partly, it was about owning the language. So, we re-played the videos of the groups presenting their campaign ideas (see previous blog post to watch). Below are the posters they produced.
However, this time, we wanted to try using pictures to sharpen and personalise those meanings. We gave people a choice of 20-30 images and asked them to choose which ones ‘spoke to them’ about person-centred care and support. Most communication, as we know, but can forget, is non-verbal. It includes gestures, facial expressions, eye contact, body language and touch, but it also includes pictures. As the adage goes, “a picture is worth a thousand words” – in some situations….
After people had chosen a picture, we asked them to share what it meant to them… (insert videos)
This proved quite powerful and was also a task that people enjoyed.
Last session’s homework
For homework, everyone had agreed to identify resources/supports for the community mapping exercise we were about to do. We shared the information provided by those not able to attend today’s meeting. This included information about the Motherwell Locality Support Service (Disability) and Making Life Easier – an online service offering advice, information and direct access to simple pieces of equipment and adaptations for people living in North Lanarkshire.
Several in the group agreed that these looked to be useful services, but questioned why they had never heard about it before – either directly, by being signposted by practitioners or through doing online searches? ‘Whose job’ was this to make sure people knew? How did we stop people being passed around the houses when they were trying to get in touch? Did we need named contacts? Why weren’t these services effectively identified through online search engines? And then there were the services people didn’t like so much or weren’t so relevant e.g. American sources of information on heart disease were potentially confusing as provided in a different context and other sources. Other sources were deemed ‘too full of jargon’ (North Lanarkshire council website), ‘too negative’ or, provided out of date information about life expectancy following diagnosis which was scary and damaging!.
Issues raised
- We want ‘trusted’ information
- We want information relevant to this client group
- Why don’t we know about some of the good stuff going on?
Everyone seemed raring to get to the community mapping!
Mapping community assets
We set out to map the assets we had locally. But what do we mean by community assets? These can be resources, places, activities, businesses or services – as identified by the people who use them in helping them stay strong and well.
We broke the group into two and asked them to use a traffic light system, writing down ‘assets’ and plotting these on large printed maps of the North Lanarkshire area:
- Green post-its for those assets they really like
- Yellow post-its for those assets they liked, but where they could see room for improvement (noting what these improvements might be)
- Red-post its for ‘the gaps’ – the ‘missing’ assets they wished were there
Both groups explored the existing assets in great depth, with people learning from each other what assets make a real difference in their lives and what types of services and activities would enhance the area. Post-it notes were place accurately on the maps to provide an accurate overview of the distribution of assets in the area.
After that we brought the two groups back together and looked at similarities and differences. Rikke expertly facilitated the discussion around what the maps were telling us. They looked quite different, and maybe one thing they were telling us were that different group members were expert about ‘their own patch’ but not others. For example, those who lived in Wishaw knew a lot more about what Wishaw has to offer than they did about Motherwell. Alison mentioned that Voluntary Action North Lanarkshire and Voluntary Action South Lanarkshire had completed a mapping exercise for voluntary organisations – with searchable info base and locator tools. We resolved to look at this next time and include this data.
As a group we also touched on how and when this information could be used – exploring issues of access; mediation; maintaining up-to-date information and responsibility for doing this. We talked about ALISS as one way of doing this. ALISS describes itself as a ‘local information system for Scotland’ for health and wellbeing resources. It’s searchable by keyword, location or within a certain mile radius that you can set. Plus everyone can add to it, describing resources in the words that they choose. Whether or not North Lanarkshire Council could produce an online map was also mentioned as a possibility worth further exploration?
Introducing approaches to improvement
We divided our group into two mixed groups of four and set them the Marshmallow Challenge. It’s described by its inventor, Tom Wujec, as ‘a design exercise that encourages teams to experience simple but profound lessons in collaboration, innovation and creativity.’
The task is simple: in eighteen minutes, teams must build the tallest free-standing structure out of 20 sticks of spaghetti, one yard of tape, one yard of string, and one marshmallow. The marshmallow needs to be on top. There are also some rules to adhere to- such as not cutting the marshmallow up or holding the structure up when the time runs out! Here’s how our two groups did!
It’s been repeated many times with different groups, revealing surprising lessons – highlighted in these summary slides: marshmallow challenge- lessons. Who tends to do the worst or best? Why? Try it yourself and see what your group finds out about itself and discuss what improves or hinders you being successful at the task!
According to Wujec, the marshmallow challenges reveals a number of lessons :
- That prototyping provides the best results – this is what nursery kids know and graduate business students and Chief Executives don’t. (According to Wujecc, kids also spend less time jostling for power?)
- Teamwork and diverse skills provides the best results – with specialised and facilitation skills leading to success
- Incentives have a negative impact if people have low skills (and don’t know about the above). If they do, the effect is reversed.
- And last, but not least, beware of hidden assumptions in our attempts – that marshmallows are light and easily supported for example
We also introduced this video ‘Leadership from a dancing guy‘ to the group ‘ by watching a movement happen’.
It’s thought-provoking and identifies certain lessons, including the importance of followers.
- A leader needs the guts to stand alone and look ridiculous
- A leader should be easy to follow
- A leader should embrace followers as equals (its’a about the movement, not you)
But leaders are also over-rated…
- It takes guts to be a first follower. It’s the first follower who transforms a lone nut into a leader!
- A follower should be easy to follow too. They need to be public as new followed emulate the first follower, not the leader.
Soon you reach a ‘tipping point’ and have a movement as more people join in and come off the fence. Eventually those who haven’t joined in will be ridiculed for being the odd ones out! ‘Watch the film and see a movement happen!’ (Personally, it reminds me of people at a wedding and going from an empty dance floor to a full one!)
We also guided the group through Approaches to improvement – this is a powerpoint presentation with notes that we created. This has key pointers of things to consider (and things to avoid). Thanks need to go to Jason Leitch, Clinical Director, Quality Unit at Scottish Government. His presentation at the National Learning Event (People at the Centre of Health and Care) on 27-28 May 2014 in Glasgow inspired much of this, although it has been adapted -so I take full responsibility for that.
In summary:
- There’s always room for improvement
- Focus on what you can do, not what you can’t
- You choose how you respond to things (take control)
- Find enthusiasts to try out new improvements on (not those who are reluctant)
- Don’t start with a large test/pilot
- Don’t try and get one person to do it all
- Measure your improvement tests to find out of its been successful – do this often and feedback your results quickly
- Strong evidence for innovation is necessary but not enough to result in its adoption – you need to win hearts and minds
- Spread the improvement- pass on the baton, find followers and new leaders
What we want to pilot/trial
Our plan had been to split the group into 2 or 3 smaller working groups to:
- generate improvement ideas that they wanted to trial;
- share with whole group and identify ‘strongest’;
- choose which ones to take forward, develop and implement.
This was to be informed by the community mapping exercise we had just completed and the introduction on how to approach improvement. We talked them through the kind of detail we hoped to get to, using a template and notes to guide this.
However, best laid plans don’t always happen! With only eight people in the group, and only three with lived experience of heart failure, the group discussed whether it should break up into two smaller groups or not? The decision was to try and attempt the first part of the task as a single group – splitting up into different groups once ideas to take forward had been chosen.
But we didn’t get past stage 1! This may have been affected by the size of the group (9), which made managing group dynamics and time more difficult. Nevertheless, we weren’t inclined to force the group past this stage as we felt we needed to let conversations happen.
Lively discussions around what we wanted to change led the group to the following improvement ideas that would require further development.
- Self-help / peer support groups (with discussion around what these would offer to people or would do e.g. should they be campaigning groups too and/or be seen by professional providers as a useful resource/ network to draw on lived experience?)
- Easy access to information/trusted information
- Activity groups plus need to be easy to find!
- Training/education of centre staff- leaflets
- Speaking to the ‘right people’ re: access, referral, time?
- Named individuals on information
- First stop shops: 18 in North Lanarkshire Council; Main Street: all local authority information, but integration=wider remit
- Group to pull information together and distribute it
- Groups have to be able to adapt to constant change
- How would we like agencies to communicate our information/condition specific information
We provided the group with a summary of ‘What we hope to achieve and potential ideas for improvement‘ generated at earlier meetings so nothing was lost! This provided a useful cross-check.
Homework
This arose from the previous activity. The group agreed to do the following as homework for the next meeting in September:
Everyone:
- Investigate the effectiveness of different search terms on line
- Collect useful resources and think about where they can go/bring back examples of websites where communication is good
- Provide a website wish list e.g. open access; it would cover lifestyle information, NHS and local authority services; a visual google map of local groups; access to a Facebook group etc…
We also discussed membership of the group. With the loss of several people with lived experience of heart failure due to ill health, we felt it would be useful to try and redress the balance with the professionals. We still hadn’t given up on trying to recruit a local GP.
Louise
- Try again to find a local GP for the group, with two possibilities…
- Try to recruit another person with heart failure or carer to the group to – aiming to find someone who is confident and would be able to slot in quite easily.
Kathie
- To investigate creating a digital map of relevant local services for the group, hosted by North Lanarkshire Council.
Everyone
- Group members were also invited to contribute to this blog. Volunteers required!
It was suggested that this could involve: sharing their own reflections on the project; sharing their personal story of heart failure and what has helped them; sharing their reflections on how person-centred the care they deliver as professionals is; anything else!
This contribution could be written, include a photo montage or be a short film.
We also agreed that it was ok to share the group member’s contact details with each other- with there some enthusiasm from a couple of members for meeting up before the next session on the 24th September 2014. This would be at our new home at South Dalziel Studios in Motherwell.
Feedback and evaluation
Of the eight group members, six gave the day a thumbs up. Two were ‘not so sure,’ hoping for more definitive outcomes and plans to take away from the day.
What went well?
- Lunch
- Good sense of developing where we are going
- Circular seating arrangement
- Sharing at the start of he day
- Have targets/vision – though lots of work still to do
- Being challenged- with different voices
What could have been better?
- Lunch
- More definite outcomes for today for some; however, majority happy with progress
What will you take away from today?
- Homework actions
- More information
- Sense of a goal and consensus
- Questions about group make up (given drop in numbers)
4 June 2014 – Second meeting of the group
Here’s our Programme for the day
Goals for the day:
- To understand person-centred care
- To understand the assets we have- and how we can optimise them and help each other
- Agree our homework and what’s next?
The importance of review, re-cap, repetition and reinforcement
Never underestimate the need to re-cap and review. We used the start of this meeting to re-state project aims, what we understood by co-production and sharing the working together agreement that the group had agreed last time along with its hopes and ambitions for this work.
This was also set within the context of the project Timetable so people could see the trajectory of this work.
So, while in the previous blog post (on meeting 1) the need to allow for time to build up relationships, learn together and establishing solid agreement was stressed, the desire from this group to move quickly to action was quite tangible! Showing them where we were as part of a project plan was, I hope quite helpful in keeping them on board and dealing with their desire to rush to action!
Repetition is also useful for dealing with concepts like person-centred care which are hard to grasp…. Or to quote the ancient Romans: Repetitio mater studiorum est, or “Repetition is the mother of all learning.”
Defining person-centred care
The concept of person-centred care and support is a slippery one! There is clearly no defined or agreed definition, with the 2014 Health Foundation publication ‘Helping measure person-centred care‘ making the connection between this and the challenges in evaluating it!
Most agree that it’s about relationships between people, however. I also like this thought from Andy Crawford, Head of Clinical Governance at NHS Greater Glasgow and Clyde that whatever ‘it’ is, ‘it’s negotiated.’
At this meeting the group shared their homework from meeting 1: their reflections on what person-centred car and support means to them; what person-centred care and support should look like. (link to flicker captures?). We also decided to share other individual’s perspectives on what ‘person-centred care’ meant as a stepping off point and chose these from The Health Foundation: a GP’s perspective; a person self-managing themselves’s perspective.
[youtube]https://www.youtube.com/watch?v=y43TLRzal44[/youtube]
[youtube]https://www.youtube.com/watch?v=x7Zu4P1qK48[/youtube]
However, we also felt it would be useful for the group to ‘own the language’ themselves and create their own version. Why? People need to feel confident in themselves about speaking about it before they can engage with or challenge others on the topic. We asked them in small groups to devise a person-centred campaign. We set the task out as following:
Purpose of campaign:
To help people know what person-centred care and support means – and what they can reliably expect of/for themselves and others.
Also consider:
- What should it say?
- How should it be presented?
- How and where could it be used?
This might be a poster campaign, radio campaign, street or viral campaign etc. It was up to each group to decide.
We provided groups with other examples to work from/be inspired by, namely: NHS Scotland’s ‘5 Must Do with Me’ areas ‘ and the Principles of Person-centred care and support developed for the Person-Centred Health and Care Collaborative to ‘help find the words and change conversations.’
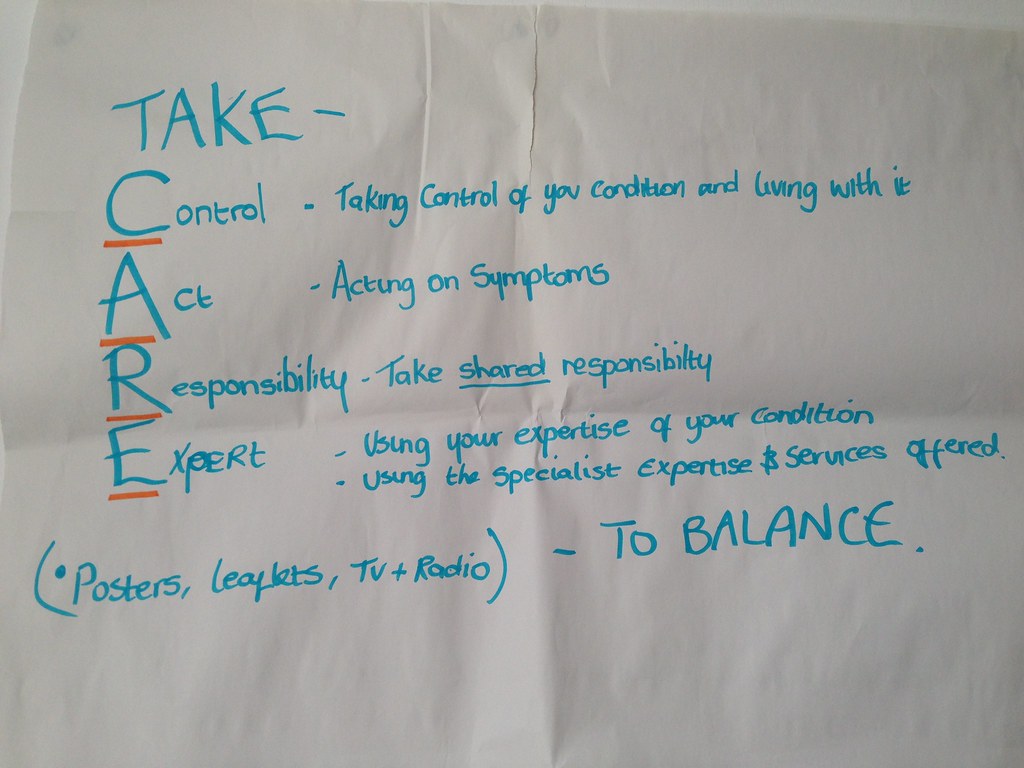
Here are the campaigns our 3 small groups came up with!
The power of positive thinking
As our ice-breaker for this meeting we asked people to speak in pairs about what keeps them strong (before moving to repeat with a new partner in the group).
Some described this as a ‘lightbulb moment’, a more appreciative approach. Feedback from people as to what keeps them strong included:
- Having goals or being determined
- A positive mental attitude
- Glass half full rather than half empty attitude
- Time to oneself/’me time’
- Music
- Doing things one enjoys eg a bit of pampering or the football or gardening
- Being loved by family/encouraged by others
- Being needed by others
- Pets
- Being pampered
- Holidays
- Speaking to others in a similar situation to myself
Communication and ‘Teachback’
“The biggest problem with communication is the illusion that it has taken place.”
(George Bernard Shaw)
The notion that effective communication is a hidden problem was introduced – people hide misunderstanding. We all worry about looking stupid and are tempted, for example, to nod along to the technician explaining what’s wrong with our computer, even though we don’t have the foggiest! Sometimes we look up the internet instead or talk to friends and get ourselves in a pickle, not knowing what information to trust or how it relates to us!
It’s also worth ‘remembering’ that half of what a person is told is forgotten and half of what they remember is misunderstood! According to some studies, 40-80% of medical information is forgotten by a patient (Kessels RP, 2003) and nearly half of the information retained is wrong (Anderson et.al, 1979)! This, and the need to check peoples’ understanding is well-illustrated by this snippet from the American TV programme, House about a genius but awkward and flawed MD.[youtube]https://www.youtube.com/watch?v=zG2DVoRP86g[/youtube]
We saw this as an opportunity to introduce ‘Teachback’ as a device that has been promoted in the NHS. Basically, it’s about professionals checking peoples’ understanding by asking them to repeat back what’s been said and, at the same time, improving their skills in being able to explain things in simple language without jargon or medicalised terms or using other tools like diagrams to help. ‘Health literacy’ after all is really about the ability to access, understand and action information!
We used a Scottish Government DVD resource (Teach back: checking understanding in consultations), created through the self management programme to illustrate this. There were no examples re heart failure, so we chose one about a woman being recommended to have an HIV test.
Interestingly, feedback form some group members on the DVD that we used was relatively negative in that they did not think that this would be an effective communication tool at a time of crisis e.g. at the point of diagnosis or raising a serious issue for the first time. In relation to heart health, our group felt it could be more effective in managing a condition over time eg going in for regular check ups. Perhaps this American example which fits this description, found through The Health Literacy Place‘s links on the Teachback method would have been better? What do you think? We’d avoided using this as earlier comments from this group had suggested they they found examples or information from other countries potentially confusing as the context was different. Furthermore, our other Keeping it Personal group had found the story of a carer from Australia who looked after her father who had dementia, harder to relate to than, say, someone’s story in Glasgow!
Finding the perfect example, is not always easy. Nenertheless, you might want to consider what can go wrong if communication is poor and Teachback isn’t used as with this example on managing your medicines, specifically warfarin.
What’s important to you (WITTY)?
WITTY is designed to help people create a personalised visual map of what’s important in their life to promote well-being. In our group we asked people to work in pairs and use a paper tool (concentric circles), placing themselves in the centre of the circle and what was important to them closer or further away from them based on their own life. This could be anything from people in their lives to pets, to social groups, places, activities and experiences that were important. This might include going to the football with friends, going for a walk by themselves or being pampered at the hairdressing salon! People can be given the option of writing on the paper circles or using props- like lego pieces (houses, people, pets etc) to represent what was important if they so chose.
The exercise was introduced by the notion that personhood covers a number of aspects (McCormack, 2004, ‘Person-centredness in gerontological nursing: an overview of the literature’)
1) Being in a social world– we are social beings,
2) Being in relation- we exist in relationships with other people,
3) Being in place– people have a context thro which their personhood is articulated,
4) Being with self– how we feel about ourselves – with how we are treated impacting on this.
The task
In pairs, people were asked to take turns using the WITTY resource
Roles:
- One completes WITTY and talks through
- One listens and reports back /summarises at the end
People are reminded that it’s ok to stop people to check for clarification/ understanding/ observe/take notes. They are asked to think about and apply the Teachback technique.
Here’s what one of the maps looked liked! (INSERT)
Following the exercise we asked for group feedback on how they found the exercise using the following questions.
- What’s the difference between asking: What’s the matter with you? to ‘What matters to you?
- How easy/difficult was it to communicate with each other in the exercise?
- How and when could you use these tools and techniques?
Here’s what they said!
- It’s broader
- Less negative
- WITTY helps reveals relationships between different things/people to help you cope.
- Much more positive!
- The general view was that it was ‘quite easy’ to have a conversation around ‘What’s important to you?’
- Good with someone I don’t know.
- Good at prioritising and sharing.
- Mapping life- shows the positives and good
- Can also show bits in life that are lacking (and help you plan for)
- Might identify lots of ‘paid’ support but not ‘natural’ ones – can then help build those up and make connections.
- Helps you open up and can help establish relationships
- May depend on who is using it -barriers may naturally go up with some eg a GP?
- Helps you be more comfortable with new services
- Need to be genuine ie. the person using the tool needs to be really interested.
- Plus, the relevance of Teachback could be seen (when maybe not before)!
There was also discussion around the fact that some people used these techniques naturally however, this was not true for all and the value of having tools to support this was agreed.
A personal example of what was important was offered by someone in our group!
- The most important people to me are my wife and my family and their wellbeing
- Cooking is important to me and
- Gardening and cycling
- Doing volunteer driving
- I’m close to my brother, sister, mother and aunt.
- Housework’s important, but it’s on the outer ring!
- What I’d like more of: holidays and meals out with friends.
WITTY was developed as part of IRISS’s project. For further information on running a workshop for what is sometimes called ‘individual asset mapping’ see the ‘Social Assets in Action’ blog. From this project a free version for use on an i-pad was developed ( iOS 6 required) with online tutorial. For more information on the WITTY app.
Moving things forward and homework for next time!
We took the opportunity to revisit 16 things identified at the previous meeting as potential actions (or future improvement activities) and asked the group:
- Have any of these already been done?
- Should any be actioned for next or next again meetings?
- Should any be parked for now (with scope to bring back later if we want)
- Are actually future improvement activities we want to consider implementing at a later stage in the project?
We split group into three smaller groups and asked to plot on a timeline, with a parking lot also available for those they wanted to discount. Here’s a picture of one of the three. The three were by no means identical.
This was very useful in showing up similarities, but also real differences of opinion in the larger group – useful for discussion and useful for identifying what things needed further clarification and work. Here’s their work in progress ‘Moving things forward‘ list as well as list of Potential Improvement Ideas – which will be developed at future meetings, with only some chosen to be taken forward.
Feedback and evaluation
As with all meetings, we ask at the end for general feedback, a gut reaction response. People are given smiley faces, not so sure and unhappy faces to hold up. We got all smiley faces with the exception of two ‘unsures.’
What went well?
- Taking stock and direction
- Good to see everyone again
- Learnt about new things eg teachback
- All mixed well
- What keeps me strong exercise and ideas.
What could have been better?
- The photos! (taken for the personal profiles)
- Be good to have a bell!
- Timings- felt that we tried to cover too much in the time for some; a 5 min warning before the end of sessions and people taking personal responsibility for listening to this (see above!)
What will you take away from today?
- Clearer about progress and what meetings are about.
- Continued sense of sharing and learning together























Looking good. Loads of information been shared already from everyone.